Die Opioidkrise in den USA gipfelte 2015 in einem starken Anstieg von Opioidabhängigen und damit verbundenen Todesfällen. Ein aggressives Marketing mit einer Opioid-verharmlosenden Strategie einiger Pharmafirmen führte dazu, dass schnell anflutende Opioide einer breiteren Patienten-klientel verschrieben wurden. In einem ersten Teil des Artikels (1) wurden der Stellenwert einer Opioidtherapie sowie das rationale und praktische Vorgehen bei einer analgetischen Therapie mit Opioiden in Bezug auf schweizerische Verhältnisse kritisch diskutiert. Im aktuellen Teil werden hierzulande zugelassene Opioide vorgestellt, Überlegungen zur Opioid-Sicherheit in der Schweiz präsentiert sowie die Eingangsfrage nach einer drohenden Opioidkrise in der Schweiz eingehend erörtert.
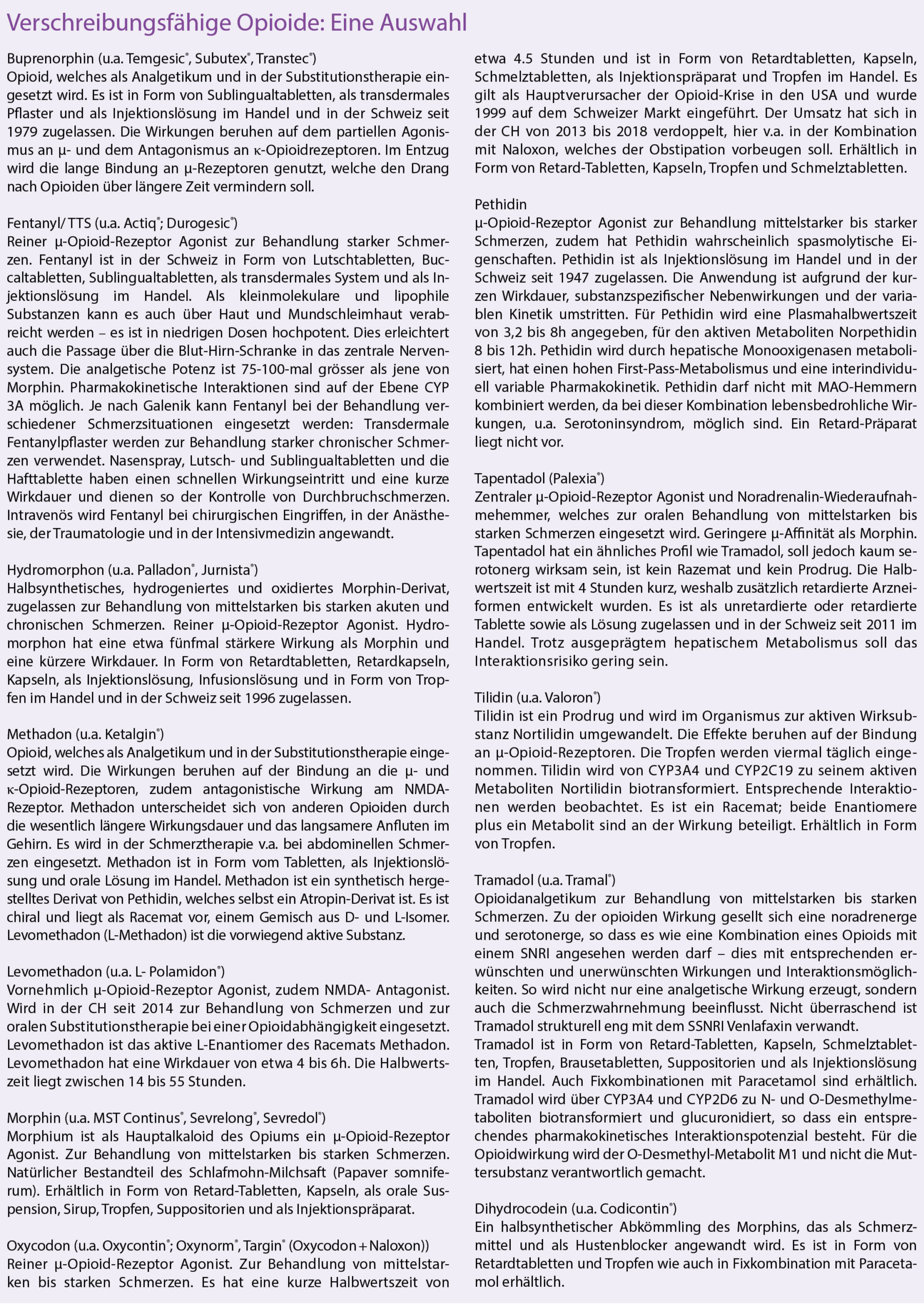
Im Hinblick auf einen angemessenen Einsatz von Opioiden unter Vermeidung von Überverordnung, aber auch Vermeidung von nicht sinnvoller Vorenthaltung von Opioiden, ist es sinnvoll, die Wirkstoffe zu kennen, die derzeit in der Schweiz zur Verfügung stehen (Kasten 1).
Droht nun der Schweiz, analog zu den USA, eine Opioidkrise?
Die Antwort vorweg: Wir wissen es nicht, haben es aber als Schmerztherapeuten in der Hand, dies zu verhindern.
Opioidverschreibungen und Opioidgebrauch nehmen auch in der Schweiz in den letzten Jahren massiv zu (2). Dies in Einklang mit anderen europäischen Ländern. Die Indikationen, für die Opioide nun vermehrt verschrieben werden, sind auch hierzulande die Nicht-tumorbedingten Schmerzzustände, obwohl eine diesbezügliche Risiko-/Nutzenabwägung nicht immer positiv ausfällt. Zwischen 2006 und 2013 verzeichnet sich in der Schweiz eine Zunahme der Verschreibung schwacher Opioide per 100 000 Personen um 13% und um 121% für starke Opioide. Unter den starken Opioiden wurde Fentanyl meistgebraucht mit einem Anstieg zwischen 2006 und 2013 um 91%, gefolgt von Buprenorphin und Oxycodon. Der höchste proportionale Anstieg in der Einnahme von Morphinäquivalenten pro 100.000 Personen wurde für Methadon (+ 1414%) und Oxycodon (+ 313%) verzeichnet. Dabei existieren starke geographische Unterschiede in verschiedenen Kantonen. Im Spitzenreiter Fribourg beispielsweise hat die Verschreibung starker Opioide in diesem Zeitraum um 270% zugenommen, im Kanton Jura um 260%, in Basel-Stadt um 219%, in Uri um 220% und in Schaffhausen um 201% (2). Übrigens zog auch die Verschreibung von Nicht-Opioidanalgetika in diesem Zeitraum rasant an: Schweizweit für Metamizol beispielsweise um 324%, NSAIDs (+ 124%). Besorgniserregend ist, dass bei den Opioiden vor allem kurzwirksame galenische Formen wie orale (+ 509%) oder sublinguale (+301%) Formulierungen häufiger verschrieben wurden.
Zum Vergleich: In den vergangenen 20 Jahren liess sich in den USA ein 14-facher Anstieg der Verschreibung starker Opioide verzeichnen. Dieser ging einher mit einem erhöhten Risiko unintentioneller Überdosierungen. In Europa war dies weniger zu beobachten und das Risiko, durch eine chronische Opioidverschreibung abhängig zu werden, wird hierzulande als gering eingestuft (3). Ausnahme bildet vor allem die Fentanyl-Überdosierung, die sich in (Ost-)Europa häufiger für Todesfälle verantwortlich zeigt. In den USA waren dies v.a. Kombinationen aus Oxycodon oder Hydrocodon und Alprazolam. Die Toten, die in den Statistiken zur Opioidkrise in den USA erfasst werden, haben in 75% der Fälle Opioide in Kombination mit Sedativa wie Alkohol, Benzodiazepinen oder Antihistaminika konsumiert. In Europa wird die Opioidkrise auch als Phänomen der ökonomischen Misere in den deindustrialisierten Gegenden der USA wahrgenommen (4).
Genau zu differenzieren ist in diesem Kontext, ob Abhängigkeit und Überdosierung durch illegalen Drogengebrauch oder im Kontext einer schmerztherapeutischen Behandlung entstanden und erfasst sind. In Europa wird bei Eintritt in eine Entzugsbehandlung Heroin von 80% der Patienten als Droge konsumiert. Dies gefolgt von Methadon (8%), Buprenorphin (5%), Fentanyl (0,3%) und anderen Opioiden (7%) (5). Heroin hat in der Schmerztherapie in Europa keinen wesentlichen Platz, so dass davon ausgegangen werden kann, dass der Grossteil von Abhängigkeitserkrankungen im Rahmen eines illegalen Abusus und nicht einer Schmerztherapie vorkommt.
Eindeutig festzustellen ist aber, dass vor allem schnell anflutende Opioide wie Oxycodon oder das Folgepräparat Oxycontin, welche neben rascher Schmerzlinderung auch stärker das zentrale Belohnungszentrum aktivieren, eher abhängig machen als retardierte Präparate – sogar Dr. House, der es besser wissen sollte, war davon betroffen. Oxycodon wurde 1919 erstmalig in der Schmerztherapie verwendet. In Europa war die Substanz schnell reguliert, nur auf Betäubungsmittelrezept erhältlich und zwischenzeitlich aufgrund erhöhter Suchtgefahr sogar vom Markt genommen. In den USA hingegen war Oxycodon ununterbrochen auf dem Markt, gefolgt vom Folgepräparat der Familie Sackler, Oxycontin. Dessen Abhängigkeitspotenzial wurde verharmlost und die Substanz intensiv beworben, immense Geldsummen flossen in aktive Bewerbung und Zuwendungen an verschreibende Ärzte. Von seiner Markteinführung 1996 bis zum Jahr 2000 hatte seine Verordnung schon um das 18-fache zugenommen. Und Drogenabhängige entdeckten, dass man die Substanz gemörsert auch intravenös verwenden konnte – was zu zahlreichen akzidentellen Intoxikationen und Todesfällen führte. Eine positive Drogen-anamnese zählt bei uns demnach auch zu den von den Leitlinien definierten Kontraindikationen für einen Einsatz von Opioiden. Nach dem Skandal um die Firma Purdue und Rekordstrafen, die sie wegen der unerlaubten Vermarktung von Oxycontin eingefahren hat, wird man in Europa kaum die gleichen Fehler machen (6). Schon aus regulatorischen Gründen wäre eine ähnliche Vermarktungspraxis hierzulande unmöglich.
Leider lesen wir momentan eine Flut an Kommentaren mehr oder weniger in der Schmerztherapie bewanderter Therapeuten, Opioide seien gefährlich, verantwortlich für eine Flut an vermeidbaren Todesfällen und man solle diese Substanzklasse komplett verbieten. Auffällig, dass diese Kommentare häufig von Therapeuten kommen, welche alternativmedizinisch arbeiten und so ihre Angebote promoten und/oder wenig mit der Behandlung chronischer und schwer betroffener Schmerzpatienten zu tun haben. Dazu ein simpler Vergleich: Antibiotika, Benzodiazepine oder Insulin sind wertvolle Medikamente, solange man sie indikationsgerecht, gezielt, wohldosiert und gemäss geltenden Therapierichtlinien einsetzt. Bei einem Zuviel oder bei unkritischer Verwendung sind diese Sub-stanzen gefährlich − dennoch würde niemand behaupten, diese Substanzen seien so riskant oder schädlich, dass man sie nicht mehr verwenden dürfe. Analog gilt für Opioide: Diese Substanzklasse ist wirksam und bei kundiger Anwendung (welche sowohl einen informierten Arzt als auch einen informierten Patienten bedingen) halten sich die Gefahren in Grenzen.
Ein häufiger Spezialfall: Die analgetische Behandlung des alten Patienten
Diese Situation stellt den Schmerztherapeuten vor grosse Herausforderungen. Demografisch bedingt suchen uns immer mehr alte Patienten im schmerztherapeutischen Setting auf. Nicht-Opioidanalgetika sind bei Alten häufig kontraindiziert oder deren Langzeitanwendung bei chronischem Schmerz nicht untersucht. Eine Übersicht über den Einsatz und die Gefahren von Nicht-Opioidanalgetika beim geriatrischen Patienten findet sich unter (7).
Opioide werden mit breiter Evidenz vor allem bei alten Krebspatienten eingesetzt. Allerdings scheinen sich die Erwartungen der Patienten an ihre Schmerztherapie zu wandeln: Heute sind ein aktiver Lifestyle mit der Möglichkeit der Teilnahme am gesellschaftlichen Leben wichtiger denn je zuvor. Viele Patienten machen in Europa bzgl. Ihres Schmerzes daher eher Zugeständnisse zugunsten einer erhaltenen Funktionalität. Transdermale Fentanyl- oder Buprenorphin-Systeme zur Schmerzcoupierung werden von diesen Patienten häufig bevorzugt.
In der Behandlung von Nicht-Karzinomschmerzen fehlen Langzeitstudien für Opioide bei geriatrischen Patienten. Sicherheit und Verträglichkeit sollten mit individueller Titration und regelmässiger Monitorisierung von Leber- und Nierenfunktion gewährleistet werden. Neuropathischer Schmerz benötigt meist höhere Opioiddosen als nozizeptiver Schmerz und besonders neuropathischer Schmerz scheint gut auf Buprenorphin anzusprechen. Als einziges Opioid ist die Elimination von Buprenorphin nicht durch eine verminderte Nierenfunktion eingeschränkt, so dass diese Substanz in der geriatrischen Patientenklientel zu bevorzugen ist. Bei anderen Opioiden sollten die Dosen ggf. verringert und auf mehrere Einzelgaben verteilt werden.
Opioide und Atemdepression: Besonders bei Patienten mit eingeschränkter pulmonaler Reserve oder bei solchen, welche mehrere zentral depressive Substanzen einnehmen, müssen Opioide sorgfältig und zurückhaltend eingesetzt werden. Auch hier bieten transdermale Systeme Vorteile (8).
Opiatsicherheit in der Schweiz
Dass sich in den USA die Opioidkrise entwickeln konnte, ist eine traurige, aber im Nachhinein nachvollziehbare Tatsache. Es stellt sich die Frage, was wir aus den gemachten Erfahrungen lernen und verhindern können, dass sich in der Schweiz gleiches wiederholt? Nehmen wir dazu drei Positionen ein: Diejenige des Arztes, des Patienten und des Gesetzgebers.
Was kann der Arzt tun, damit nicht zu viele Opioide verschrieben werden?
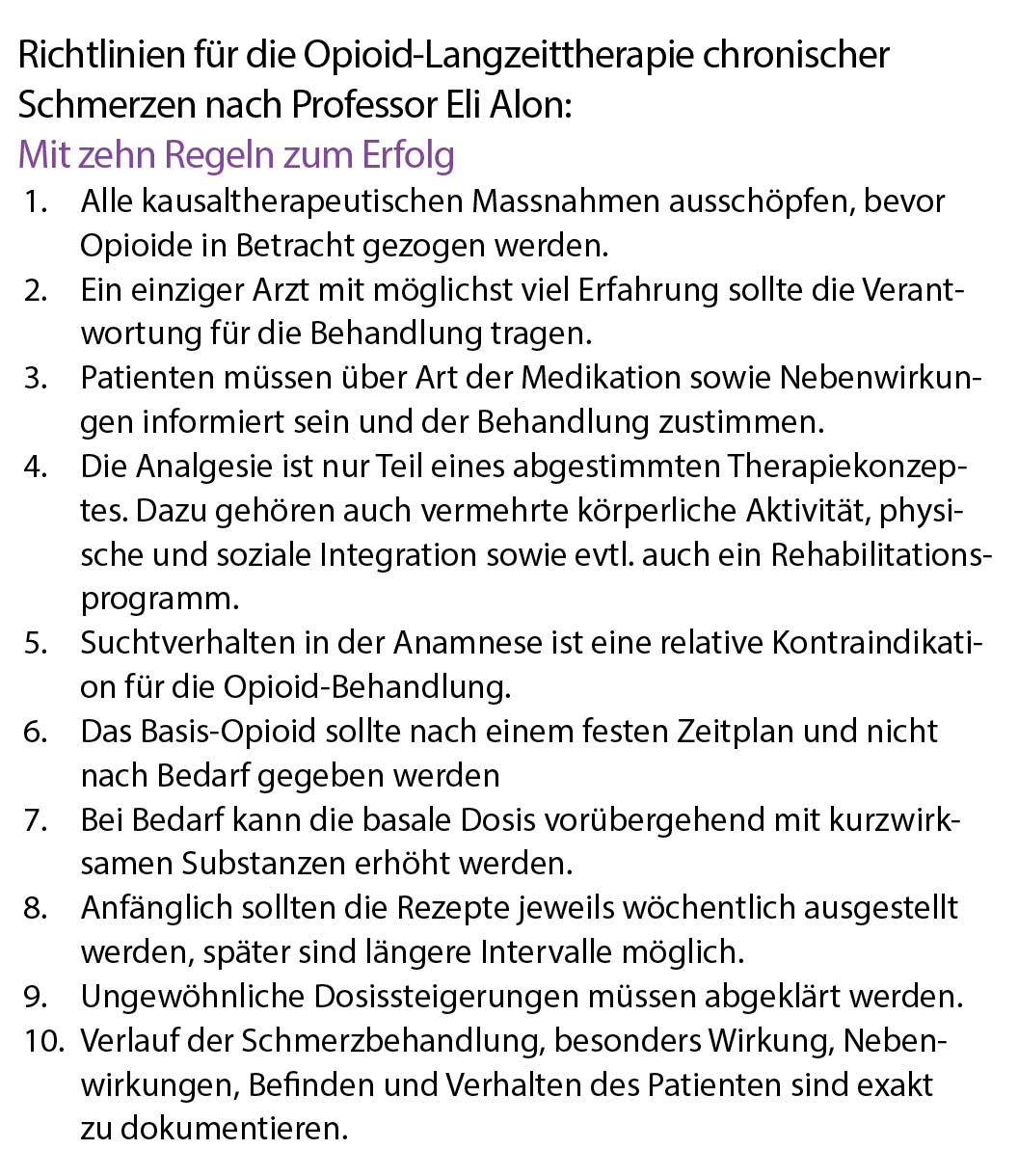
Der informierte Arzt stellt die Indikation für Opioide eng, d.h. nach geltenden Therapieempfehlungen und nach Ausschöpfung aller verfügbaren und sinnvollen Optionen, welche pharmakologische und nicht-pharmakologische Therapien umfassen. Er vereinbart mit dem Patienten klare und erreichbare Therapieziele sowie regelmässige Konsultationen zur Reevaluation. Retardpräparate, welche nach einem fixen Dosierungsschema eingenommen werden, sind schnell anflutenden Galeniken vorzuziehen. Diese sollten als Reservemedikation Schmerzspitzen vorbehalten sein. Über potenzielle unerwünschte Wirkungen und Risiken muss der Patient ausführlich aufgeklärt werden, dies inklusive des Suchtrisikos. Es wird Kontakt zu mitbehandelnden Ärzten gesucht und vereinbart, in wessen Hand die Pharmakotherapie liegt (Kasten 2).
Was kann der Patient tun, damit er nicht abhängig wird?
Wichtig ist, dass Behandlungsziele zu Beginn der Behandlung abgemacht werden, dies möglichst schriftlich. Ist die dann durchgeführte Behandlung nicht zielführend – die eingesetzten Opioide beispielsweise nicht ausreichend schmerzlindernd – soll ein neues Therapieregime angewendet werden.
Der Patient muss realistische Therapieerwartungen haben – bei langjährigen schweren Schmerzerkrankungen ist eine völlige Schmerzfreiheit ein unrealistisches Ziel. Schmerzreduktion, Funktionalitätsverbesserung oder manchmal auch nur eine bessere Schmerzverarbeitung sind oft die realistischen Ziele.
Zudem darf der Patient nicht an verschiedenen Orten Medikamente beziehen, sich nicht von mehreren Ärzten Medikamente verschreiben lassen. Der behandelnde Arzt ist darüber genau zu informieren, wer bisher in die Therapie einbezogen ist und welche Massnahmen getroffen wurden. Offene Kommunikation und eine intakte Patient-/Arztbeziehung sind mandatorisch.
Und der Patient darf, was selbstverständlich sein sollte, keine illegalen Substanzen zusätzlich konsumieren. Auch über einen Cannabis-Konsum sollte der Behandler informiert sein.
Was kann der Gesetzgeber tun, damit Opioide nicht übermässig verschrieben werden?
Die Opioidverschreibung in der Schweiz ist klar geregelt und findet eine optimale Balance zwischen der kontrollierten Verschreibung und problemloser Erhältlichkeit für medizinische Zwecke. Erleichternd wäre, wenn Informationen zur Verschreibung auf einer Patientenkarte gespeichert würden, aus denen ersichtlich ist, was der Patient im individuellen Fall schon von wem verschrieben bekommen hat – nicht nur in Bezug auf Opioide, sondern auch auf andere, möglicherweise interagierende Substanzen, von denen der Verschreiber wissen sollte. Eine erhöhte Transparenz könnte hier zu verbesserter Arzneimittel- und damit Patientensicherheit führen. Pharmazeuten und Versicherer arbeiten schon lange an entsprechenden Lösungen, welche v.a. aus datenschutzrechtlichen Gründen bisher nicht realisiert sind.
Fachärztin für Klinische Pharmakologie und Toxikologie FMH
Fachärztin für Anästhesie FMH, Schmerzspezialistin SGSS
Leiterin Sprechstunde Medikamente in Schwangerschaft und Stillzeit
Oberärztin Psychiatrische Klinik Königsfelden
Postfach 432
5201 Brugg
antje.heck@pdag.ch
Facharzt für Anästhesiologie FMH, Schmerzspezialist SGSS
Professor für Anästhesiologie und Schmerzmedizin an der
Universität Zürich
Praxis für Schmerztherapie
Arzthaus Zürich City
Lintheschergasse 3
8001 Zürich
eli.alon@arzthaus.ch
Die Autoren haben in Zusammenhang mit diesem Artikel keine Interessenskonflikte deklariert.
1. Heck A, Alon E: Einsatz von Opioiden aus der Sicht des Schmerztherapeuten (Teil 1). Der informierte arzt 2020;10(4):10-12
2. Wertli M et al: Changes over time in prescription practices of pain medications in Switzerland between 2006 and 2013: an analysis of insurance claims. BMC Health Serv Res. 2017 Feb 27;17(1):167
3. Hess B et al: Relevance and Application if Opioids in the Treatment of Chronic Pain in Switzerland- a National Survey. PRAXIS 2015;104 (11):557-63
4. Daniel Ryser 16.10.2018. Wir haben keine Opioid- Krise. Wir haben eine Krise der Ignoranz. Republik.ch
5. INCP Annual Report 2018
6. Zeit online: Oxycontin. Die Pillendreher. Nr 49/ 2017
7. Heck A, Alon E: Nicht-Opioid-Analgetika in der Geriatrie. Der Informierte Arzt 2019;9(9):33-37
8. Pergolizzi J et al: Opioids and the management of chronic severe pain in the elderly: consensus statement of an International Expert Panel with focus on the six clinically most often used World Health Organization Step III opioids (buprenorphine, fentanyl, hydromorphone, methadone, morphine, oxycodone). Pain Pract. 2008 Jul-Aug;8(4):287-313.